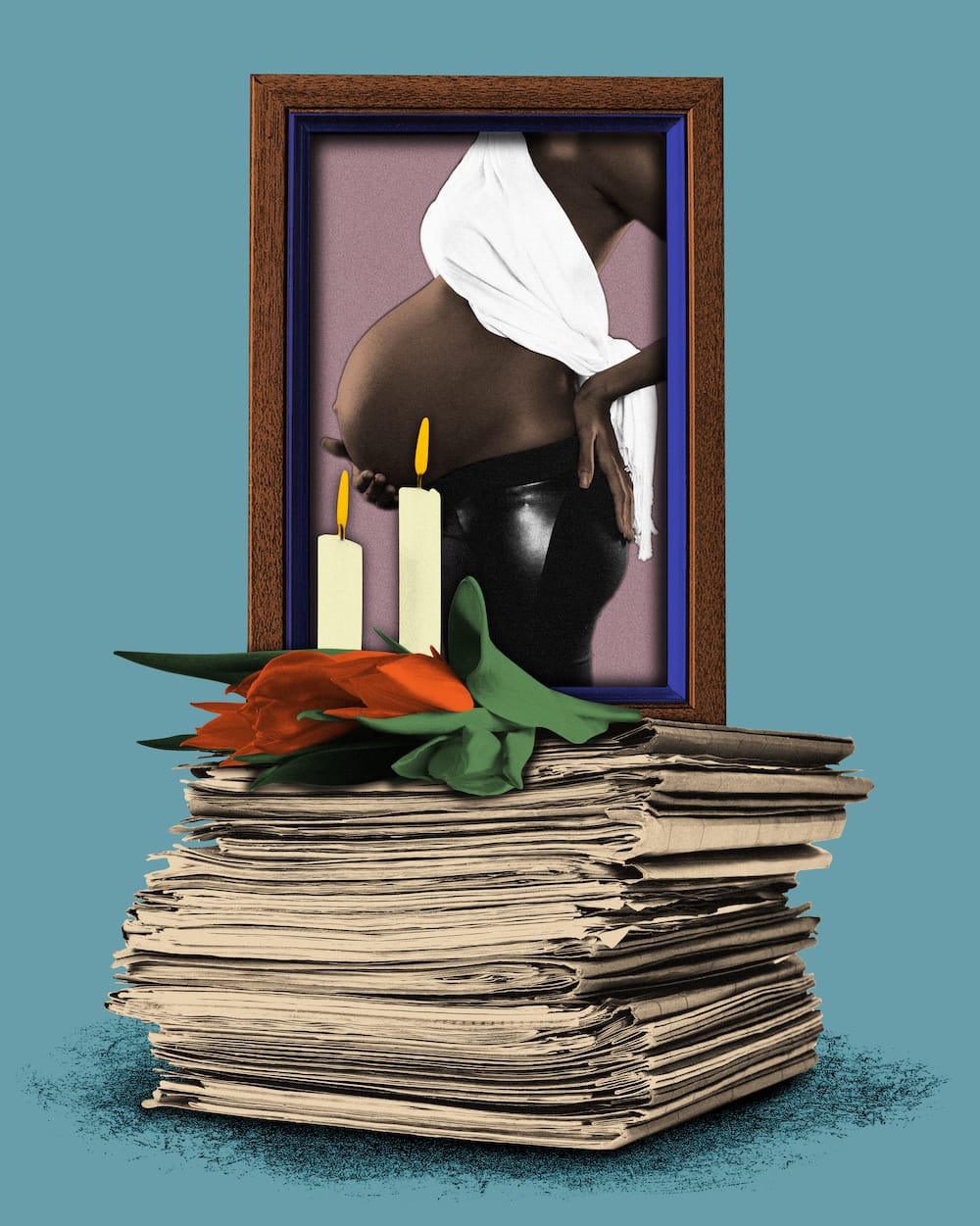
Two Years On, The Biden-Harris Effort To Reduce Maternal Mortality Remains—A Start
Maternal mortality is shockingly high in the U.S. What exactly is being done about it?
The Persistent is available as a newsletter. Sign up here to get it delivered to your inbox.
The U.S. presidential election has been, to put it mildly, head-spinning. A CNN debate nobody could stop talking about. An assassination attempt. A late-in-the-race drop-out. A conversation on X plagued by tech troubles. Standing ovations at the DNC. It’s certainly kept us on our toes.
This might explain, in part, why the White House’s sprawling update on efforts to combat the U.S. maternal health crisis—released on July 10—hasn’t been top of mind.
The progress report follows up on 2022’s Blueprint for Addressing the Maternal Health Crisis, a comprehensive endeavor from the Biden Administration, spearheaded by Vice President Kamala Harris, to lower America’s dismal maternal mortality rates. The report was something of a first—56 pages of dense research and policy suggestions, calling on Congress to invest millions.
It couldn’t come a moment too soon.